CMS
CMS finalized a rule that implements reductions to Medicaid disproportionate share hospital (DSH) payments. The new rule will result in a reduction of $8 billion in DSH payments annually from fiscal year 2024 to 2027. Previously, MACPAC has expressed concerns that these reductions could adversely affect some safety net hospitals as they estimated it would reduce DSH allotments by about 54%.
In-network Findings
- New Fair Health analysis found that in-network care increased from 84% to 90%. In particular specialties that are more commonly associated with out of network care (anesthesiology, emergency rooms, etc.) saw larger increases in proportion of in network billing
- One potential source of the change is the No Surprises Act, which protects consumers from surprise bills. A good summary of the current process can be found here. Overall providers and amounts higher than median amount have won a majority of the disputes in the first half of 2023.
Weight Loss Drugs
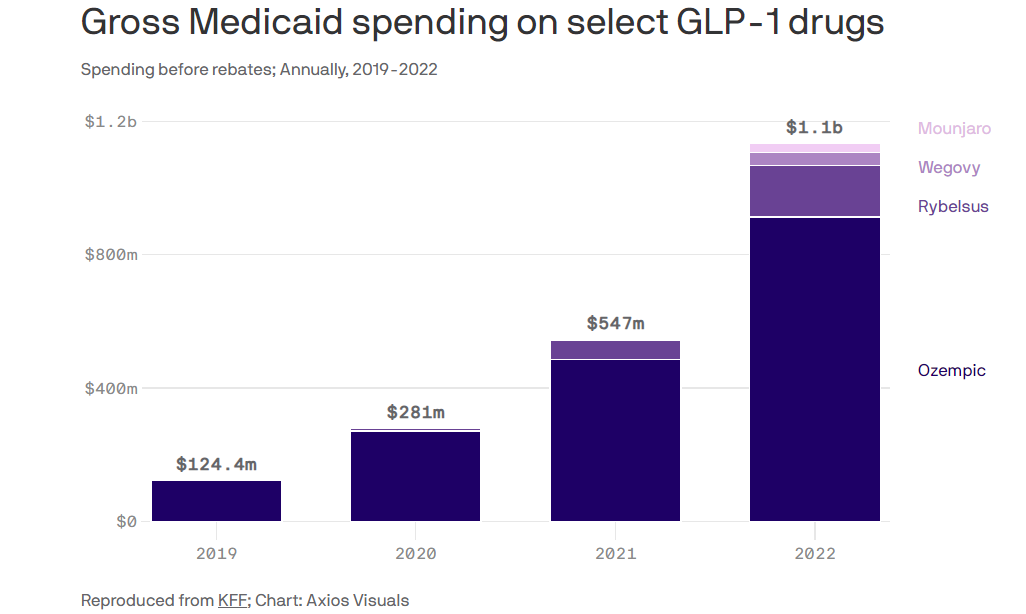
Axios reported that an increasing number of state employee benefit plans and Medicaid programs are instituting cost savings measures to protect against high-cost weight loss (GLP-1) drugs. Spending has dramatically increased on these drugs putting increasing pressure on state budgets.
Research You Can Use
The Center for American Progress released estimates of post-negotiation Medicare drug prices for the 10 drugs selected for negotiation. The researchers estimates that price reductions could range from $30 for NovoLog Flexpen to $6,548 for the cancer drug Imbruvica.

